|
연간정보 서비스
상품코드
1349830
두경부 편평상피암(HNSCC) : Tumour DeckHead and Neck Squamous Cell Carcinoma (HNSCC) - Tumour Deck |
||||||
두경부(H&N)암의 주요 표적은 입술 점막, 인두, 후두, 부비동 등 구강에서 발생하는 종양입니다. 이들 종양의 95% 이상이 편평상피암입니다. 구강암, 인두암, 후두암, 인유두종바이러스(HPV) 비관련 중인두암의 가장 흔한 원인은 담배와 알코올 사용 장애입니다. 두경부암, 특히 담배와 알코올로 인한 두경부암 환자는 두경부, 폐, 식도, 방광 및 이러한 발암 물질에 노출된 다른 부위에 원발성 종양이 동시에 발생하여 이차 원발성 신생물이 발생할 위험이 있습니다.
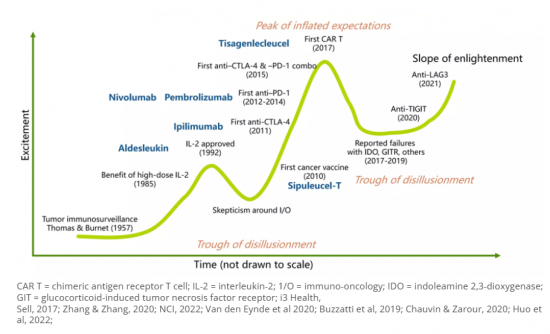
전이성 두경부암은 특히 방사선과 화학요법을 포함한 선행치료로 병이 진행된 후의 치료가 문제입니다. 지난 4년간 면역요법이 승인되고, 두 개의 PD-1 억제제가 재발 전이 치료제로 승인되면서 큰 활기를 띠고 있습니다. 현재 임상시험이 진행 중이고, 이것이 최종 치료제로 전환되고 있습니다.
두경부 편평상피암은 암세포만으로 구성된 것이 아니라, 종양세포가 미세환경의 다양한 컴포넌트와 상호작용하는 역동적인 생태계입니다. 이 생태계에는 면역세포, 암 관련 섬유아세포(CAF), 암 줄기세포(CSC), 혈관계, 인유두종바이러스(HPV)와 같은 바이러스 인자가 포함됩니다. 이러한 컴포넌트 간의 상호 작용과 상호 작용을 이해하는 것은 효과적인 치료 전략을 개발하는 데 필수적입니다.
진행기 종양의 발생률이 상대적으로 높은 것은 HNSCC 종양에서 초기 환자의 증상이 제한적이거나 초기에서 진행기로 빠르게 진행되는 것과 관련이 있을 수 있습니다. 따라서 전이를 조기에 발견할 수 있는 종양 바이오마커의 개발이 필수적입니다. 종양 마커는 이차 예방에 중요한 역할을 합니다. 종양 마커는 생화학적 및 면역학적 표현을 사용하여 종양의 분화를 정량화할 수 있습니다. 현재 FDA는 28개의 바이오마커를 체외에서 확실한 시험을 거쳐 임상 사용을 승인했습니다. 그러나 HNSCC의 진단 및 예후를 위해 FDA가 승인한 단백질이나 돌연변이 마커는 아직 없습니다.
다제 병용요법을 받은 국소 진행성 HNSCC 환자의 50% 이상이 완치를 목표로 한 치료를 마친 후 3년 이내에 재발 및 전이가 발생합니다. 현재 조기 발견을 위한 효과적인 스크리닝 방법이 없기 때문에 상당수의 환자가 진행된 상태에서 진단을 받고 있습니다.
세계의 두경부 편평상피암(HNSCC) 시장에 대해 조사했으며, 시장 현황과 함께 증례수의 동향, 환자 동향, 경쟁 제품 시장 포지셔닝, 시장의 기회 등을 제공하고 있습니다.
목차
제1장 주요 요약
제2장 두경부 편평상피암(HNSCC)의 개요
- 두경부 편평상피암(HNSCC)의 정의, 증상, 병인, 병인
- HNSCC에서 분자 변화
제3장 두경부 편평상피암(HNSCC)의 정의와 진단
- 진단용 바이오마커
- 진단 알고리즘
제4장 두경부 편평상피암(HNSCC) 역학
- 국가별 이환율
- HNSCC의 국가별 단계적 분류
제5장 두경부 편평상피암(HNSCC)의 치료 실천
제6장 두경부 편평상피암(HNSCC) 승인된 표적 치료
- 표적치료의 개요
- 두경부 편평상피암(HNSCC)에서의 미충족 요구
- 질병 재발 및/또는 전이율이 높다
- HPV 양성 HNSCC와 HPV 음성 HNSCC의 치료 전략에 구별은 없다.
- 현재 새로운 표적치료의 과제
제7장 파이프라인 임상시험
- 두경부 편평상피암(HNSCC) 파이프라인 상황의 개요와 분석
- 분자 표적치료의 임상 개발
- 임상시험에서의 주요 분자와 결과
- 주요 의약품 승인과 발매 타임라인
제8장 제III상자산
- 임상시험과 결과
- 제II상자산
- 임상시험과 결과
제9장 제I상자산
- 임상시험과 결과
제10장 두경부 편평상피암(HNSCC) 파이프라인 초기 단계 분자
제11장 두경부 편평상피암(HNSCC) 파이프라인 비임상 분자
제12장 의사/KOL 인풋
- 미국, EU, 일본의 4명 KOL로부터의 인사이트
- 두경부 편평상피암(HNSCC)의 주요 이벤트
- 승인된 표적치료의 확대
- 새로운 시행 가능한 목표 작성
제13장 두경부 편평상피암(HNSCC) 시장 예측-2033년
- 주요 약제별 시장 예측과 환자 점유율
제14장 부록
KSA 23.09.27Head and Neck (H&N) cancers primarily targets tumors originating from the oral cavity, including the mucosal lip, pharynx, larynx, and paranasal sinuses. More than 95% of these tumors are squamous cell carcinomas. The most common causes for oral cavity, hypopharynx, larynx, and Human Papillomavirus (HPV)-unrelated oropharynx cancers are tobacco and alcohol use disorders. Patients with H&N cancers, particularly those caused by tobacco and alcohol, risk synchronous primary tumors and developing second primary neoplasms in the H&N, lung, esophagus, bladder, and other sites exposed to these carcinogens.
"Metastatic head and neck cancer is a challenging disease to treat particularly after disease progression on prior therapy, which usually includes radiation and chemotherapy. Over the last 4 years, we've seen the big excitement with immunotherapy being approved, with 2 PD-1 inhibitors approved in the recurrent metastatic setting. We're seeing this moving now to the definitive therapy setting with trials that are accruing."
Head and neck squamous cell carcinoma is not solely composed of cancer cells but is rather a dynamic ecosystem where tumor cells interact with various components in their microenvironment. This ecosystem includes immune cells, cancer-associated fibroblasts (CAFs), cancer stem cells (CSCs), vasculature, and viral factors such as human papillomavirus (HPV). Understanding the interactions and crosstalk between these components is essential for developing effective treatment strategies.
The relative higher incidence of advanced stage tumours could be related to limited symptomatology in patients with early stage or swift progression from early to advanced stage in HNSCC tumours. Up to 40% of cN0 necks harbor occult metastatic disease. Hence, developing tumour biomarkers to detect metastasis at early stage is essential. Tumour markers play a significant role in secondary prevention. Tumour differentiation can be quantified using biochemical and immunological representation as tumour markers. Currently, the FDA has approved 28 biomarkers after robust in vitro tests for clinical use. However, there is no protein or mutation marker approved for diagnosis or prognosis in HNSCC by the FDA
Mellalta Meets: Predictive Biomarkers of Checkpoint inhibitors
Predictive Biomarkers of Checkpoint inhibitors
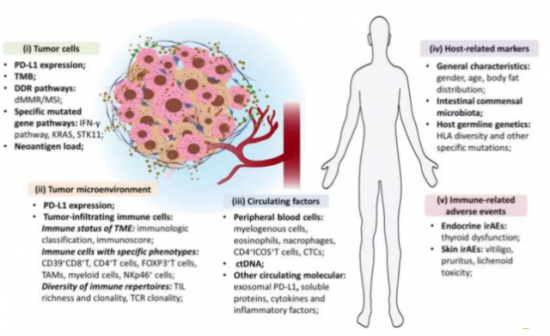
Source: Bai et al, 2020.
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Current Treatment Landscape
The current standard of care for locally advanced (LA) HNSCC and recurrent/metastatic (R/M) HNSCC involves a combination of treatment modalities, including surgery, radiation therapy (RT), and chemotherapy.
For LA HNSCC, the primary treatment modality is often a combination of surgery and RT. In some cases, multimodal approach is considered in which chemotherapy may also be administered concurrently with RT to enhance its effectiveness.
For R/M HNSCC, the treatment options are more limited. Systemic therapy, which includes chemotherapy and targeted therapy, is the mainstay of treatment. Chemotherapy drugs such as cisplatin, carboplatin, and 5-fluorouracil are commonly used. Targeted therapies, such as cetuximab (an anti-EGFR monoclonal antibody), may also be used in combination with chemotherapy.
Immunotherapy has emerged as a promising treatment option for R/M HNSCC. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, have shown significant efficacy in improving overall survival in patients with R/M HNSCC.
Mellalta Meets Immunotherapies in HNSCC
"Management of early-stage locoregional HNSCC primarily rests on a combination of chemotherapy and radiation therapy. However, the therapeutic trajectory becomes intricate for patients experiencing local or regional recurrence due to radiation field overlaps. Additionally, the management of recurrent or second primary HNSCC has become more complex due to the increased incidence of HPV-associated HNSCC compared to non-HPV HNSCC. This change in disease profile has led to a wider range of treatment options available to practicing oncologists, further complicating the decision-making process."
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Current Unmet Needs
- High rate of disease recurrence and/or metastasis and poor treatment outcomes severely affect long term survival: Over 50% of patients with locally advanced HNSCC who receive multimodal approached develop recurrent or metastatic disease within 3 years of the completing curative-intent treatments.
- Early detection of HNSCC is crucial for better treatment outcomes: Currently, there is a lack of effective screening methods for early detection, leading to a significant number of cases being diagnosed at advanced stages.
- No distinction in treatment strategy for HPV-positive and HPV-negative HNSCC which produces significant morbidity: HPV-positive and HPV-negative HNSCC distinctly differ genetically, they are treated in much the same way, an approach that produces significant morbidity. For patients with advanced-stage HPV-positive HNSCC, the 5-year survival rates are 75% to 80%, whereas fewer than 50% of patients with HPV-negative disease survive for 5 years.
- Diverse cases of Potential ICI resistance mechanisms in R/M HNSCC, which necessitates that many molecular targeted agents be tested in combination with ICIs
"Use of immunotherapy in the treatment of [HNSCC] is still evolving, with a continued unmet need for first-line regimens that provide durable clinical benefit with tolerable safety, further research is needed to determine the utility of dual immunotherapy as a treatment option for [HNSCC] and identify novel biomarkers to predict benefit with immunotherapy."
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Key Takeaways
- Radiotherapy plus concomitant chemotherapy for fit patient's with unresected LA SCCHN (stage III-IV) has been shown to improve 5-year absolute survival by 6.5% compared with locoregional treatment alone.
- Despite of Cisplatin-Associated Toxicities, Cisplatin remains the radiosensitizer of choice for the majority of patients with locoregionally advanced head and neck cancer.
- Cetuximab is the only targeted therapy that has been proven effective for the treatment of HNSCC in both the LA and R/M settings. The incorporation of cetuximab not only expanded the range of treatment options in the past decade but also encouraged the investigation of many other targeted therapies in this tumor type.
- The current standard of care (SOC) in the second-line treatment of HNSCC typically results in an ORR of approximately 10-18%. There is room for improvement in the effectiveness of existing treatments.
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Questions Answered:
- How can anti-PD-1/L1 therapies improve outcomes for patients with locally advanced HNSCC? Which combination strategies involving PD1-based therapies can drive change in recurrent/metastatic HNSCC?
- How can Merck Group's IAP antagonist xevinapant change the treatment paradigm for locally advanced HNSCC?
- How do oncologists view the role of Adlai Nortye's anti-PI3K agent buparlisib in the treatment of PD-1-refractory HNSCC?
- What are the key challenges and opportunities in the development of novel therapies for HNSCC, according to KOLs?
- Which companies are best placed to exploit the approach of novel IO-doublet regimens in HNSCC?
Table of Content
1. Executive Summary
- 1.1. Summary of future trends
- 1.2. Potential opportunities to explore.
- 1.3. Drivers/barriers for entry
- 1.4. What's new in HNSCC.
2. Head and neck squamous cell carcinoma (HNSCC) Overview
- 2.1. Head and neck squamous cell carcinoma (HNSCC) definition, symptoms, etiology, Pathogenesis
- 2.2. Molecular Alterations in HNSCC
3. Head and neck squamous cell carcinoma (HNSCC) Definition & Diagnosis
- 3.1. Diagnostic Biomarkers
- 3.2. Diagnostic Algorithm
4. Head and neck squamous cell carcinoma (HNSCC) Epidemiology
- 4.1. Incidence rates by countries
- 4.2. Stage specific cases of HNSCC by countries
5. Head and neck squamous cell carcinoma (HNSCC) Treatment Practices
- 5.1. Current treatment practices
- 5.2. Treatment algorithms
- 5.3. Summarized version of NCCN and ESMO treatment guidelines
- 5.4. Acceptable endpoints for accelerated approval?
6. Head and neck squamous cell carcinoma (HNSCC) Approved Targeted Treatments
- 6.1. Quick overview of targeted therapies
- 6.2. Unmet Needs in Head and neck squamous cell carcinoma (HNSCC)
- 6.3. High rate of disease recurrence and/or metastasis
- 6.4. No distinction in treatment strategy for HPV-positive and HPV-negative HNSCC
- 6.5. Challenges with the Current Emerging Targeted Therapy
- 6.6. To be Continued…
7. Pipeline clinical trials
- 7.1. Head and neck squamous cell carcinoma (HNSCC) pipeline landscape overview and analysis
- 7.2. Clinical Development of Molecular Targeted Therapy
- 7.3. Key molecules in clinical trials and results
- 7.4. Timeline of key drug approvals and launches.
8. Phase III Assets
- 8.1. Clinical trials and results
- 8.2. Phase II Assets
- 8.3. Clinical trials and results
9. Phase I Assets
- 9.1. Clinical trials and results
10. Head and neck squamous cell carcinoma (HNSCC) Pipeline Early-Stage Molecules
- 10.1. Phase I and Phase I/II molecules
- 10.2. Mechanism of action, trial dates, and topline results
11. Head and neck squamous cell carcinoma (HNSCC) Pipeline Non-clinical Molecules
- 11.1. Pre-clinical molecules
- 11.2. Mechanism of action, catalyst dates, and events
12. Physicians/KOLs Input
- 12.1. Insights from 4 KOLs in the US, EU, and Japan
- 12.2. Key Catalyst Events in Head and neck squamous cell carcinoma (HNSCC)
- 12.3. Expansion of approved targeted therapies
- 12.4. Creation of new actionable targets
13. Head and neck squamous cell carcinoma (HNSCC) Market Forecast -2033
- 13.1. Market Forecast and patient share by key drugs
14. Appendix
(주말 및 공휴일 제외)